Sleep Apnea

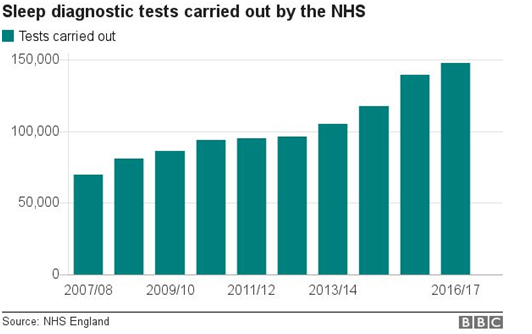
An ‘apnoea’ is defined as а lack of airflow in the mouth for at least 10-15 seconds. Sleep apnoea is a common but serious disorder where regular breathing during sleep is interrupted, thus reducing the overall quality of sleep. Because of this, it can have many negative long term consequences. In England, 1 million people are thought to suffer from sleep apnoea, but just 10-25% of these are aware they have it. Over the past years, the amount of sleep diagnosis done in the UK has doubled, indicating the increasing presence of sleep apnea.
Types of sleep apnoea
Obstructive sleep apnoea (OSA) – this is the more common form and is a result of blocked airflow during sleep, usually when the soft tissue at the back of the throat collapses during sleep. An increased risk of OSA is associated with: age, obesity, enlarged tonsils, frequent alcohol consumption, smoking, overbite and a large neck circumference. In summary – breathing movement happening BUT no airflow
Central sleep apnoea – caused by problems in the brain failing to properly signal the muscles used for breathing. This type of sleep apnoea can occur with conditions like heart failure, brain tumors, brain infections and stroke. In summary – no airflow AND no breathing movements
Mixed apnoea – a combination of both OSA and central apnoea at the same time
Hypopnea – a reduced (not stopped) airflow during at least a 10-15 second period
Predisposing factors
-
Restriction in size of the mouth cavity (mandibula, maxilla)
-
Increased size of soft tissue volume e.g. fat deposits around the upper airway, enlargement of the tongue (macroglossia), enlargement of the soft palate (back of mouth roof), etc.
-
Hormonal factors e.g. more testosterone, absence of progesterone (menopause), endocrine disorders (e.g. hypothyroidism)
-
Genetics (e.g. facial asymmetry, receding jaw)
-
Loss of muscle tone in the throat (due to an aging)
-
Swollen tonsils
How OSA happens

Normally, when you breathe in, air flows in through your mouth and throat, then down the windpipe to the lungs. Each time that you breathe in, negative suction pressure is created that pulls the soft tissue in your mouth and throat inward. The muscles in the throat respond by pulling the soft tissue outward, so that the airway is kept open. When you sleep, it’s normal for these muscles to relax slightly, but still not enough to block the airway. In people with OSA, their mouth and throat muscles relax too much, causing the tongue to drop on to the roof of the mouth and press against the back of the throat. This completely blocks the flow of air into the lungs. In turn, the person wakes up gasping for air then falls back asleep and this cycle continues through the night and can happen many times.
In general, the progression over time to OSA develops in the following way:
Snoring sometimes -> Snoring habitually -> UARS -> Sometimes hypopnea -> OSA
Upper airway resistance syndrome (UARS) – condition where muscles in the throat and airway relax too much and reduce the diameter of the airway, resulting in ‘laboured breathing’ (think breathing through a straw). This causes micro-awakenings at night that in turn cause fatigue and daytime sleepiness. This condition often precedes sleep apnoea or occurs along with insomnia.
Symptoms

Adults:
● Snoring and/or gasping for air during sleep
● Morning headaches and daytime fatigue
● Bruxism
● Night sweats
● Memory loss and reduced cognition
● Difficulty losing weight and increased appetite
● Acid reflux
● Frequent urination at night
● Personality changes and mood swings
● Dry mouth
● Impotence
● Restless legs syndrome – involuntary leg movements during sleep
Children specific:
● ADHD
● Aggressive behaviour
● Frequent coughs or colds
● Bed wetting
● Growth inhibition
Signs
If you have concerns about OSA, then the first step is to check in with your dentist, and they will take a look for the common signs.
Dentists will look for:
-
Cracked/worn teeth – grinding/clenching the teeth (bruxism) is more common in people with sleep apnoea (as common as 1 in 4). Bruxism is often caused by stress or anxiety. Over time this causes tooth sensitivity and can even cause tooth damage.
-
Jaw pain – chronic pain disorders like TMD are associated with sleep apnoea, causing pain from opening or moving the jaw bones. TMD stands for temporomandibular joint disorder and occurs when there are problems with the face muscles and jaws, causing the hinge connecting the upper and lower jaw to not work properly.
-
Enlarged tongue and/or high tongue level – increased likelihood of airflow blockage
-
Mandibular tori – a condition where bone growth occurs on the inner side of the lower jaw (below the tongue). They can either be harmless or cause some discomfort if the growth continues.
-
Teeth crowding
-
Large tonsils/uvula – these may contribute to the blocking of the airway
-
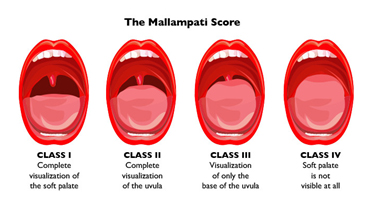
Mallampati score of 3 or 4 – this is a simple test used to roughly predict the presence of OSA by looking at how visible all of the structures in the mouth are
If your dentist believes you may have OSA they will refer you to a certified sleep specialist that will diagnose sleep apnoea through a review of family and medical history, a physical exam and a sleep study.
Sleep Physicians look for:
-
A BMI of over 30kg/m2 – obesity is related to OSA due to larger deposits of fat tissue around the neck being able to block the airway
-
Neck circumference > 43cm for men; >40cm for women
There are 2 types of tests that can be made by a sleep physician to diagnose sleep apnoea:
Polysomnography – a night is spent at the hospital, hooked up to equipment that monitors the heart, lung and brain activity, breathing patterns, limb movements and blood oxygen levels while sleeping. The patient can either have a full-night study, being monitored for the whole night, or a split-night study where they’re monitored during the first half of the night and, if diagnosed with OSA, are then given a CPAP machine for the remainder of the night to assist sleep.
Home sleep apnoea testing – under certain circumstances the sleep physician will provide the patient with a version of the polysomnography that can be carried out at home. It will usually measure airflow, breathing patterns, limb movements, snoring and blood oxygen levels.
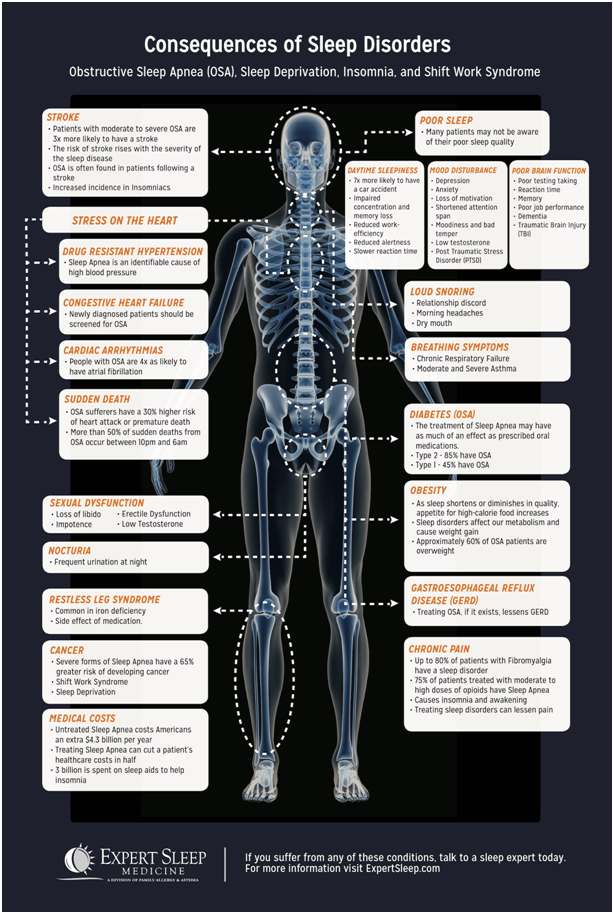
Consequences
If left untreated, sleep apnoea can lead to serious health conditions such as:
-
High blood pressure
-
Heart disease
-
Stroke
-
Diabetes
-
Sleepiness, fatigue obviously
-
Impaired memory and concentration
-
Problems with associations, problem solving
-
Creativity loss
-
Mood swings, anxiety, depression
-
Motor coordination difficulty
-
Pain in muscles, joints, headache
-
Impaired immune system
-
Metabolic syndrome
-
Road traffic or work-related accidents
-
Arrhythmia
-
Lung hypertension
Ways of treatment
Lifestyle
This is the very first thing that should be addressed when tackling sleep apnoea, because in many cases a person’s lifestyle factors can be what creates a bigger predisposition to development of sleep apnea. The following lifestyle changes can be addressed if they apply to you:
-
Weight loss – losing weight can improve or eliminate symptoms of sleep apnoea if the patient is overweight or obese. This is mainly due to a reduction in neck size and therefore having less tissue around the throat to block the airway. Weight loss is unlikely to make a difference however in patients with a narrow nasal passage or airway.
-
Quitting alcohol and cigarettes – alcohol relaxes the throat muscles and can cause snoring or collapse of the airway, while smoking may increase the severity of sleep apnoea through changes in the sleep arousal mechanisms and inflammation of the upper airway.
-
Positional therapy – a behavioural strategy to treat the way the patient sleeps, as some patients have sleep apnoea primarily when sleeping on their back. It may involve wearing a special device around the waist or back when sleeping.
Continuous Positive Airway Pressure (CPAP) Machine
The most commonly used treatment. The machine forces continuous airflow through the nose to prevent the airway from collapsing when muscles relax during sleep. The result is a continuous oxygen level through the night. The downside is that many people that are prescribed to wear the machine can’t tolerate it for various reasons and seek an alternative treatment instead.
Oral Appliance Therapy
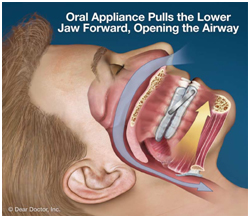 There are 2 types of devices that can be used: a mandibular repositioning device and a tongue retaining device. Mandibular repositioning devices reposition the lower jaw forward and down slightly to keep the airway open while asleep. Tongue retaining devices hold the tongue in place in order to prevent it from pressing on and blocking the airway. These are a highly effective and non-invasive option for sufferers of sleep apnoea. They fit similar to a sports mouthguard, so are comfortable and portable.
There are 2 types of devices that can be used: a mandibular repositioning device and a tongue retaining device. Mandibular repositioning devices reposition the lower jaw forward and down slightly to keep the airway open while asleep. Tongue retaining devices hold the tongue in place in order to prevent it from pressing on and blocking the airway. These are a highly effective and non-invasive option for sufferers of sleep apnoea. They fit similar to a sports mouthguard, so are comfortable and portable.
Surgery
Several different types of surgery can be performed to treat OSA:
-
Maxillomandibular advancement (MMA) – the bones of the upper and/or lower jaw are repositioned to relieve airway obstruction, and the attached throat airway muscles are suspended in an anterior position so that the soft tissue tension is increased. The result is an enlargement of the entire upper airway. The procedure is challenging because positioning needs to be very precise, but the long term success rate is generally very high.

-
ENT-surgery (ear, nose, throat):
-
Turbinectomy – removal of some or all of the turbinates (small bony structures that occur in the nose)
-
Septoplasty – correction of a deviated septum (the cartilage in your nose that divides the nostrils), therefore straightening out the nose
-
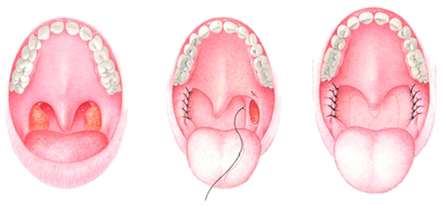
UPPP – removal of excess throat tissue such as the uvula, tonsils and part of the soft palate to make the airway wider. Structures are then placed to prevent the collapse of the airway. UPPP can cause a big improvement for patients with snoring, as there is less reverberation of the soft palate with the back of the throat
-
Somnoplasty – surgical treatment for snoring, where heat energy is used to modify the tissue of the uvula, soft palate, nose or tongue by inserting a needle probe at the site of obstruction and passing a small current
-
Soft palate implants – minimally invasive procedure that can help snoring and mild sleep apnea. Three polyester rods are placed into the soft palate, which stiffens it and makes it less likely to make contact with the back wall of the throat during deep sleep
-
Hyoid advancement – this is a small bone in the neck where the tongue base and throat muscles attach. Patients with sleep apnea often have a large tongue base that makes contact with the back of the throat during sleep. A minimally invasive procedure places stitching around the hyoid bone, repositioning it anteriorly, and suspends it to the front of the jaw bone. The result is an expansion of the airway, with collapse prevented. This procedure has had major success
-
Tracheostomy – creates a passageway for air to get to the lungs directly from the trachea in the neck, therefore bypassing any potential obstructions in the upper airway. A permanent tracheostomy is an option in morbidly obese patients with obesity hypoventilation syndrome
Prescription medication
Medication is not a primary treatment method for sleep apnoea but can help patients manage their symptoms. Below are some medicines that may be prescribed to patients to alleviate the symptoms of OSA and improve wakefulness:
-
Modafinil
-
Armodafinil
-
Solriamfetol
